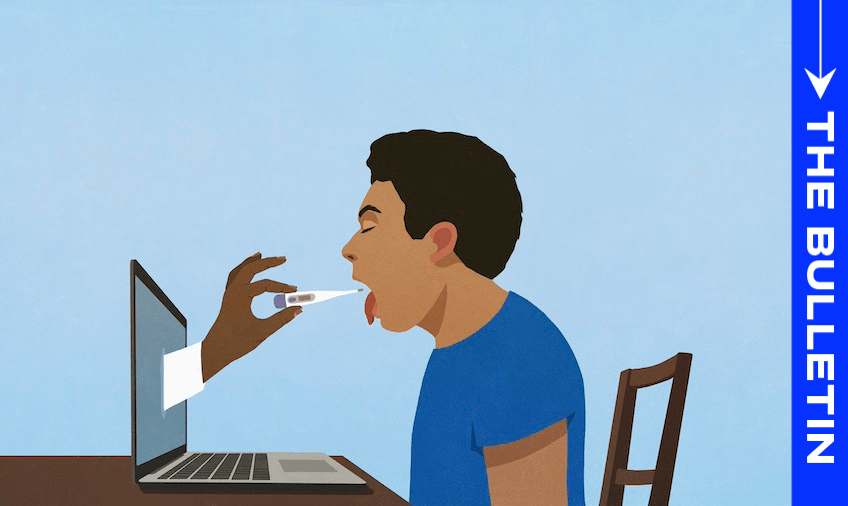
The government is betting big on remote healthcare, announcing a new 24/7 telehealth service. But virtual treatment is not always a substitute for IRL care, writes Catherine McGregor in today’s extract from The Bulletin.
To receive The Bulletin in full each weekday, sign up here.
Overseas doctors may staff new service
Online GP appointments are set to become a lot more commonplace with the announcement of a new 24/7 nationwide telehealth service. Health minister Simeon Brown says it will play a vital role in addressing GP waiting times, though doctors staffing the service may not necessarily be based in New Zealand. Speaking at Monday’s announcement, he said that “many of them will be from New Zealand” but “some of them may be GPs registered in New Zealand, but working offshore, able to support that service”, The Post’s Anna Whyte and Rachel Thomas report (paywalled).
How popular is telehealth currently?
While telehealth services saw a surge in uptake during the pandemic, usage has since receded. Research last year by the Health Quality and Safety Commission found that the proportion of GP appointments conducted via video call has never exceeded 20%, reports Mariné Lourens in The Press (paywalled). A Royal New Zealand College of General Practitioners survey showed “48% of respondents never use video call when engaging with patients, while 25% never use patient portals. The main reason cited for not offering remote consultations was a lack of demand from patients.” The numbers have no doubt increased since that survey was conducted in 2022, particularly in areas where practices have been forced to introduce telehealth services due to GP shortages.
Not a panacea, GPs warn
Many GPs are keen supporters of telehealth, arguing that any tool which gives patients better access to healthcare has to be a positive. On the other hand, Dr Bryan Betty, chair of General Practice New Zealand (GPNZ), tells Lourens he thinks the benefits of telehealth have been “oversold”. It “tends to be useful for singular and semi-acute problems, but there is an inherent danger that [the doctor doesn’t] get a comprehensive picture of the patient’s health”, he says.
Writing in The Conversation, health academic and part-time Northland doctor Kyle Eggleton cites research demonstrating how telehealth can encourage unsafe medical practices such as increased prescribing, and is unsuitable for a range of more complex health issues. “These end up getting pushed back onto face-to-face doctors to be managed acutely or in emergency rooms, thereby increasing the burden at these points of care,” he writes.
Funding for more primary care doctors and nurses
Along with the telehealth service, Monday’s announcement included a new two-year programme training for up to 100 overseas-trained doctors to allow them to work in primary care, reports the NZ Herald. The government will also help fund the recruitment of 400 graduate nurses a year by GP practices and other non-hospital providers through incentives of up to $20,000 per placement. “This helps attract essential healthcare staff where they’re desperately needed, particularly in rural areas,” Brown said. The announcement also includes a performance-based $285 million uplift for general practice over three years, starting from July 1.
Labour leader Chris Hipkins said that while “of course” he’d welcome more GPs, the health minister had dropped the ball on bigger-picture issues like illness prevention and early detection. He said the government had made the situation worse by cutting free prescriptions and underfunding the pharmacy-operated minor ailments service.