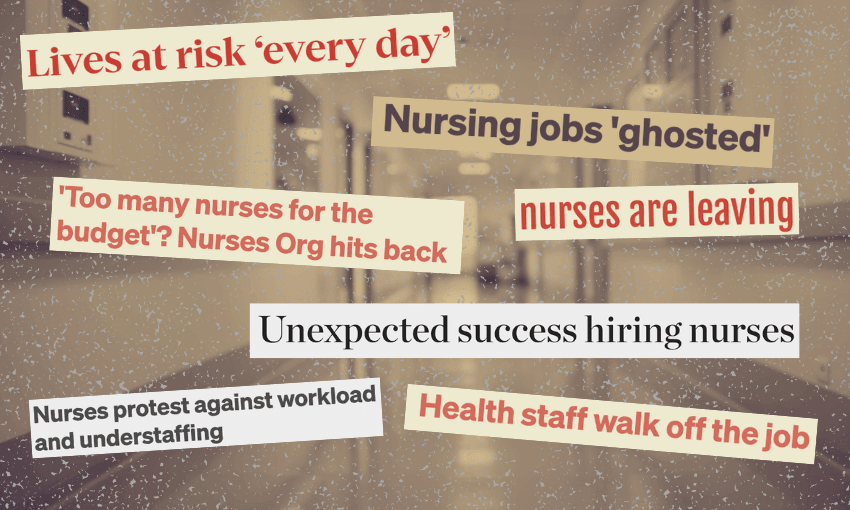
Te Whatu Ora/Health NZ has blamed a forecast $1.7bn deficit on ‘over-recruiting’ of nursing staff. But the nursing union says there’s still an ‘acute need’ for more. What’s going on?
After months of escalating concern over “significant overspending”, on Tuesday Te Whatu Ora released hundreds of pages of internal documents that shed further light on its financial state, specifically how hiring more nurses than it could afford was driving a substantial deficit. After years – and even decades – of nurses saying the health system was in crisis due to chronic understaffing and underfunding, how could there suddenly be “too many nurses”? And does “too many” for what’s been budgeted just mean there simply hasn’t been enough funding? Figuring it all out is not a simple task, but we’ve done our best to bring you this timeline.
April-August 2022
Health minister Andrew Little says New Zealand hospitals are around 4,000 nurses short. The nurses union says the sector is at breaking point. Little announces “a suite of targeted measures” to address the shortage.
April-July 2023
National, then in opposition, announces its plan to incentivise more people to train as nurses. Nurses rally around the country to demand action over a chronic staffing shortage, which by this time has grown to 4,800, based on Te Whatu Ora estimates. The Labour government launches a major plan to address shortages across the healthcare sector.
March 2024
On March 19, finance minister Nicola Willis writes to health minister Shane Reti concerned about early signals of an operating deficit at Te Whatu Ora. She says when Treasury officials met with Te Whatu Ora’s board a few weeks earlier, “the board did not seem across the detail of the issue”.
On March 21, a briefing to health minister Shane Reti from Te Whatu Ora chief executive Margie Apa says “expenditure is tracking outside budget expectations” in six areas, including “internal personnel over-recruiting, specifically nursing”. This growth in numbers is attributed to new graduate nurses, with more than 1,200 employed over the December/January period, but no corresponding reduction in outsourcing costs (ie the use of agency nurses).
Te Whatu Ora’s monthly financial update for March continues to predict a surplus.
April 2024
Te Whatu Ora confirms that hospitals have been asked to save more than $105m by July. Apa says successful recruitment “means we can reset the staffing in our hospitals, with less reliance on contingent or temporary staff. It also means staff can, and should, take leave”. Reti says he has been assured that “none of these cost-saving measures will impact the level of care patients receive”.
May 2024
An aide-memoire from Te Whatu Ora’s acting chief executive Dale Bramley to Reti reveals a “significant deterioration” in finances, with the agency $245m in the red for April. It’s “mostly explained by an underlying spending problem of about $100 million each month, most of which stems from nursing FTE [full-time equivalent] and additional hours paid”.
Bramley said that nursing headcount had increased by 2,886 from June 2023 to March 2024, and nurses “tell us that engagement and having the resources they need has improved”.
Further “cost controls” will be put in place, says Bramley, including an “immediate pause of organisation-wide recruitment, including CCDM uplifts”, but this could be overridden by senior staff “for clinical and safety considerations”. (CCDM is “care capacity demand management”, essentially a staffing safety system that identifies how many nurses are needed in a ward at any one time. As Phil Pennington at RNZ puts it, the instruction was essentially to apply the brakes to raising capacity at a time of rising demand, heading into winter.”
The aide-memoire warns that “additional and tighter controls will lead to some increased negative sentiment from parts of our workforce and representative groups”.
The nurses union, NZNO, releases “genuinely alarming” numbers that say over the course of 2023, more than a quarter of nursing shifts in public health wards were below target staffing numbers, and some wards operated below safe staffing levels nearly all of the time.
The union surveys members on the Te Whatu Ora cuts. “Overwhelmingly, they said the cuts will impact negatively on what is already a very difficult working environment,” says NZNO chief executive Paul Goulter. “Their key concern is that understaffing is already chronic and at crisis level, and that cuts to services will exacerbate that situation.”
June 2024
A “cost controls update” from Apa to Reti on June 7 says in the context of nursing, “given the substantial increases in FTE for 2023/24, little to no growth is affordable for 2024/25 and in some areas reductions will be needed”.
Later in the month, in another briefing to Reti, Apa says, “In filling roles over the last 24 months, the Care Capacity Demand Management (CCDM) method for rostering nurses became uncoupled from affordability. Our preference is to uncouple CCDM from views of what constitutes safe staffing. Workforce is only one of a range of variables that impact patient safety and how safe staff feel at work to practice…. Our intention is to manage back to budget through attrition although the leaving rate for nurses has also fallen.” In short, the intention is to scale back nurse numbers by not replacing those who leave the workforce.
Te Whatu Ora confirms a recruitment pause for non-patient-facing hospital roles, but says the frontline won’t be affected. NZNO says Te Whatu Ora is also freezing the hiring of graduate nurses into the hospital system. Te Whatu Ora denies this. Apa tells RNZ, “it is true we won’t have as many hospital-based roles as we have in previous years because we are about 2,000 nursing FTEs ahead of where we planned to be”.
July 2024
In response to “serious concerns around oversight and overspending”, Reti sacks the entire board of Te Whatu Ora, appointing board chair Lester Levy as commissioner. Asked by media about the details of the overspend – “is it new nurses or is it back-office staff?” – Reti says, “It’s a combination of things. It is back-office staff, as we’ve mentioned, but it’s also outsourced personnel.” Asked the same thing, Apa focuses her comments on nurses.
Nurses rally outside Thames Hospital to protest staff shortages. Several nurses working in hospitals tell The Spinoff that there are never enough of them to provide safe patient care. The Spinoff reports on how many overseas nurses who move to New Zealand don’t plan to stick around.
August 2024
RNZ reports that one in four recent nurse graduates remain unemployed, and Reti says nurse shortages remain in areas such as mental health, critical care and midwifery.
Further illustrating that figuring out many nurses “short” we are is not a simple equation,
Reti tells Stuff that current nurse vacancies number in the hundreds, Levy says it’s 1,000, but publicly available data suggests the correct number is 2,700, according to Stuff. Staff walk off the job at Waikato Hospital amid recruitment concerns.
September 2024
The coroner rules on the “preventable” death of a woman at Waikato Hospital’s ED in 2023, saying the ED was five nurses short at the time, a ratio “far lower than recommended”. Te Whatu Ora says nurse numbers have increased in the months since, but a nurse at the hospital says patients’ lives remain at risk “every day”.
Nurses at a number of different hospitals tell RNZ of unsafe staffing levels, with staff who go on leave, get sick or quit in many cases not being replaced.
Reti tells the NZNO conference that “of all the challenges the health system is facing, workforce is the greatest”, and that there are still nursing shortages in “community care, rural hospitals, in mental health, critical care and maternity care”.
A briefing from Te Whatu Ora to the health select committee says its forecast deficit has risen from $1.4bn to $1.76bn. The spend on nurses had dropped by about $40m from June to August. The total spend on nurses for the year to July 2024 was almost $5 billion, not much more than the figure for the previous year.
October 2024
Health NZ releases hundreds of pages of internal documents from the previous months that shed further light on the agency’s financial state (many of which are mentioned above).
Levy tells Morning Report that more than 3,000 nurses were hired beyond Te Whatu Ora’s budget. He won’t say whether or not they’re needed for safe medical care, but says a clinical patient and safety review has been commissioned. “In an ideal world we would increase our productivity so we get the best of the resources we have,” he says.
In an interview with Nine to Noon, NZNO chief executive Paul Goulter says “there are still acute needs for additional nurses”. “The budget is just a number plucked out of the air, it’s a political choice number,” he says. “What we’re dealing with is what patients actually need.”